Case Study - Eli the Golden Retriever

We would like to present Eli, a friendly 9-year-old male neutered Golden retriever diagnosed with an interesting neurological condition through successful collaboration between general practice, Vet Oracle Teleneurology and specialist referral hospital.
Case Summary
Eli started showing difficulties to walk on slippery surfaces summer 2022. This slowly progressed over ~6 months to difficulties to get up and bunny hopping when running. He was, however, not particularly painful. He was initially presented to Emma Parkinson at Carrick Veterinary Group in Chesterfield. After inconclusive routine hip and stifle X-rays and a NSAIDs trial, Emma rapidly sought advice on the Vet Oracle Teleneurology platform, run by Nicolas Granger.
Examination, Diagnosis and Possible Treatment
Emma uploaded videos of Eli’s gait through the VetOracle Teleneurology platform for Nicolas to review. The platform is well suited for advice based on videos, and this is especially useful for neurological cases. Eli demonstrated an unusual gait whereby he would progressively stiffen up soon after starting to exercise; he had generalised weakness evidenced by difficulties flexing the hips and extending his stifles during the swing phase of the gait. His breathing was also rapidly laboured. This was altogether puzzling because Eli’s gait could not be linked to more common gait anomalies caused by hip dysplasia or ataxia caused by degenerative myelopathy.
We discussed via the platform a possible myopathy secondary to hypothyroidism or Cushing’s pseudomyotonia (this is a rare myopathy characterized by persistent muscle contraction during a voluntary effort) and Emma thoroughly ruled out Cushing’s disease and hypothyroidism. We concluded that advanced testing was needed.
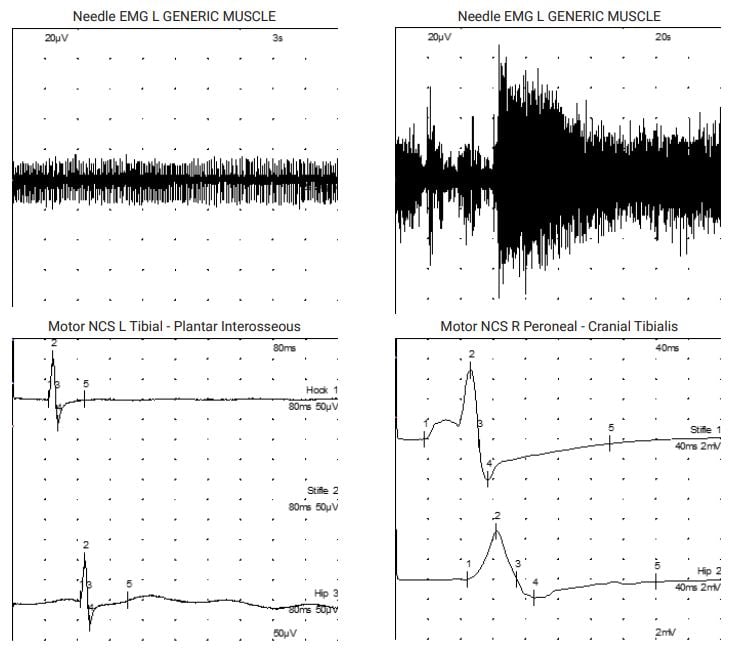
This led to referral to Thomas Mignan – specialist neurologist at Dovecote Veterinary Hospital. Thomas found the pelvic limb withdrawal reflexes decreased and absent patellar reflexes, therefore confirming our suspicion of a neuro-muscular condition. Electrophysiological testing revealed myotonic discharges and complex repetitive discharges in several muscles throughout both the pelvic and the thoracic limbs. Motor nerve conduction studies revealed markedly reduced compound muscle action potentials of the sciatic nerve but also ulnar nerve, altogether suggesting a peripheral neuropathy. Nicolas Granger was then invited to help with performing peripheral nerve biopsies. Muscle biopsies were consistent with denervation atrophy and the peroneal nerve biopsy (analysed through a collaboration with the Royal Veterinary College) revealed marked axonal loss and degeneration, with numerous axonal sprouts attempting but failing to regenerate and resulting in an axonal neuropathy.
In dogs with neuro-muscular weakness, muscle and nerve biopsies are routinely done by neurology specialists and offer the possibility to screen for inflammatory conditions: in particular polymyositis, which is treatable with corticosteroids, as much as the better known immune-mediated polyarthritis. In Eli’s case, unfortunately, the condition was a degenerative disease of the peripheral nerves. There is a laryngeal paralysis and polyneuropathy complex seen across several dog breeds[1]; some have a late-onset form, also known as geriatric onset laryngeal paralysis polyneuropathy[3]. Recently, a genetic variant has been identified in several breeds[3], such as Retriever dogs, although Golden Retrievers were only found with one abnormal copy of the mutant variant (i.e. heterozygous). Eli’s ‘ageing’ neuropathy is slightly different because he did not exhibit marked signs of laryngeal paralysis, but rather subtle gait changes that progressed over ~6 months before visiting the vet. In ageing dogs, mobility issues are often attributed to osteoarthritis.
Geriatric onset laryngeal paralysis polyneuropathy comes with a major risk of developing aspiration pneumonia and respiratory compromise. In a study[5], 94% of seventy-six owners of Labrador Retrievers with late-onset laryngeal paralysis described their dog’s quality of life as impaired by the condition. Luckily, Eli did not seem to be primarily affected by the laryngeal paralysis, although he had some mild features of this.
The presence of myotonic discharges on EMG was uncommon for us and is a feature of Cushing’s myopathy, but can occur sporadically alongside other neuro-muscular conditions. Thanks to Emma’s testing, metabolic and endocrine causes for this neuropathy were ruled out.
Currently, there is no definitive treatment for axonal degenerative polyneuropathy in ageing dogs. This is not a painful condition, as Eli’s owner noticed, and is fortunately only slowly progressive. Eli is managed with physiotherapy and encouraged to exercise regularly, two years into his diagnosis.
Here, we present an example of a case where the disease is admittedly progressive, but very slowly, thereby allowing the dog to continue to live with a good quality of life. This is a great example of team collaboration within CVS to reach a diagnosis and as such allow creation of an individualised treatment plan for the patient and owner. We do hope that Eli continues to do well!
References
[1] GOLPP|College of Veterinary Medicine at MSU. [(accessed on 7 September 2020)]
[2] A CNTNAP1 Missense Variant Is Associated with Canine Laryngeal Paralysis and Polyneuropathy.
[3] Letko A, Minor KM, Friedenberg SG, Shelton GD, Salvador JP, Mandigers PJJ, Leegwater PAJ, Winkler PA, Petersen-Jones SM, Stanley BJ, Ekenstedt KJ, Johnson GS, Hansen L,
Jagannathan V, Mickelson JR, Drögemüller C.Genes (Basel). 2020 Nov 27;11(12):1426. doi: 10.3390/genes11121426.
[4] Late-onset laryngeal paralysis: Owner perception of quality of life and cause of death.
[5] Sample SJ, Stilin A, Binversie EE, Baker LA, Hardie RJ.Vet Med Sci. 2020 Aug;6(3):306-313. doi: 10.1002/vms3.240. Epub 2020 Jan 25.
[6] Canine inherited motor and sensory neuropathies: an updated classification in 22 breeds and comparison to Charcot-Marie-Tooth disease.
[7] Granger N. Vet J. 2011 Jun;188(3):274-85. doi: 10.1016/j.tvjl.2010.06.003. Epub 2010 Jul 16.
